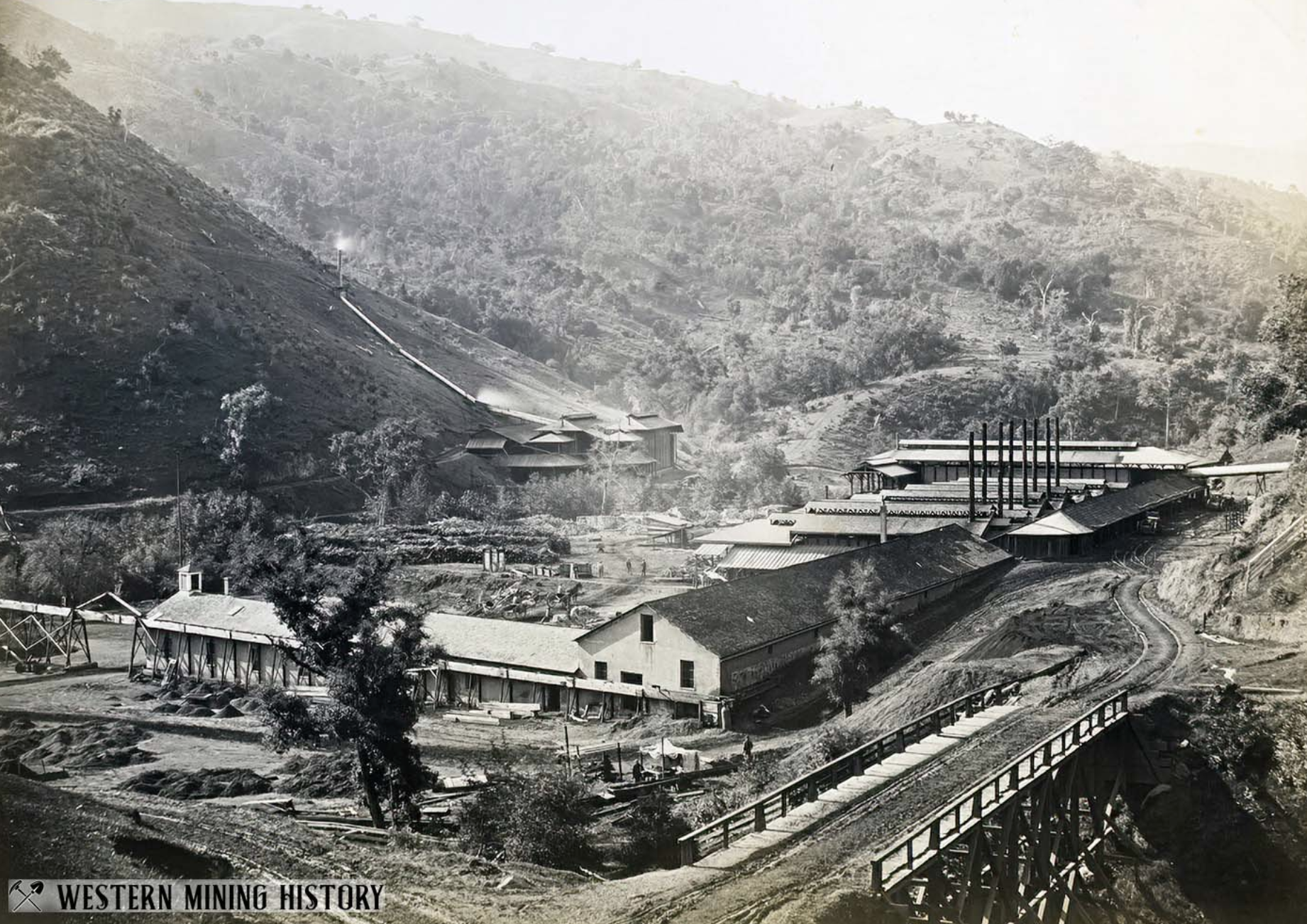
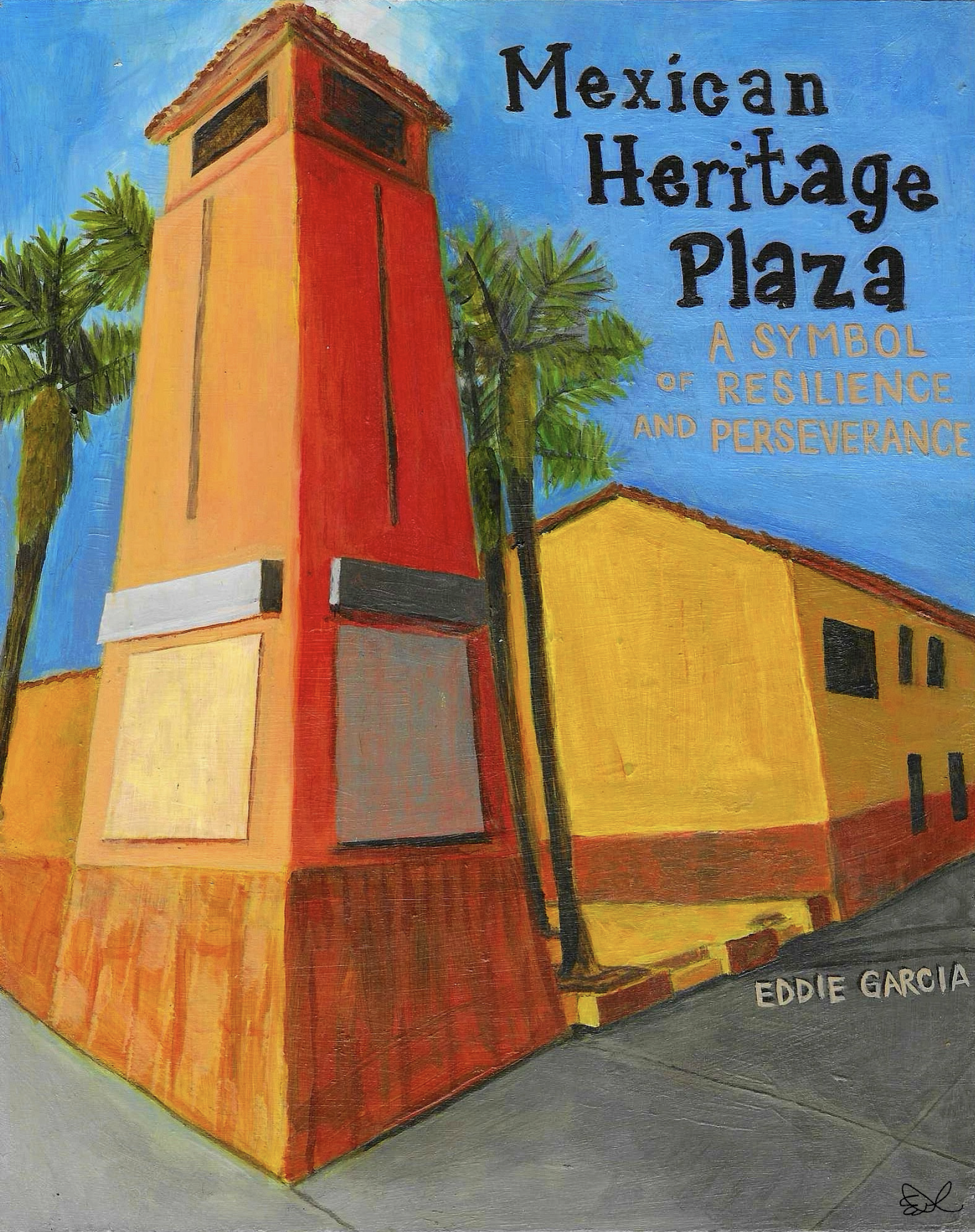
Photos L-R Clockwise: Avena Barbata, Eastern Santa Clara Valley Hills, Book Cover, New Almaden Mines ca. 1863 (image courtesy of westernmininghistory.com)
***
Chapter 4
Avena Barbata
This period of trial led to what may have been the earliest ethnic Mexican-organized labor activities in U.S. history.
~ Stephen J. Pitti, Author, The Devil in Silicon Valley
***
During the rainy season, avena barbata, also known as slender wild oat, is one of the natural grasses that blanket the green hillsides on the eastern slope of Santa Clara Valley. Before industrialization and the growth of Silicon Valley, this species of tall grasses swayed in the wind on hillsides and the valley floor as well.
During the dry season, the plant’s seeds fall to the ground, disappear into the soil, and become dormant. Some seeds can remain underground for three years before sprouting after the rains, growing to a height of up to four feet.
Slender wild oats are not native to the Santa Clara Valley or California. They originate from Asia and the Mediterranean Basin. According to botanists, the strain found in the Santa Clara Valley has the same genetic makeup as avena barbata, native to southwestern Spain.
The grass is also common in the Mexican states of Sonora and Sinaloa. Scientists speculate that Mexican settlers and ranchers introduced avena barbata to the valley in the 18th and 19th centuries to feed cattle and other livestock.
Green florets hang on the tips of a few branches that hold the seeds of the slim grass. When the wind flows through a field of avena barbata, unharvested seeds of the wild grass fly wide and far, settling into the soil below.
Botanists consider it an invasive species that outcompetes native grasses in the valley. Over the course of nearly 250 years, the slender wild oat has become more common in the Santa Clara Valley than native species.
Today, the eastern hillsides turn a lush green soon after a heavy rain. Although modern-day Silicon Valley is an endless landscape of asphalt, cement, and squat tilt-up buildings that serve the high-tech industry, avena barbata is everywhere.
During the spring, one can see tall grass on median strips, unkempt yards peeking through cyclone fences, and on open lots. Today, hiking trails in the Eastern hills cut through fields of avena barbata, gently undulating in a light springtime breeze.
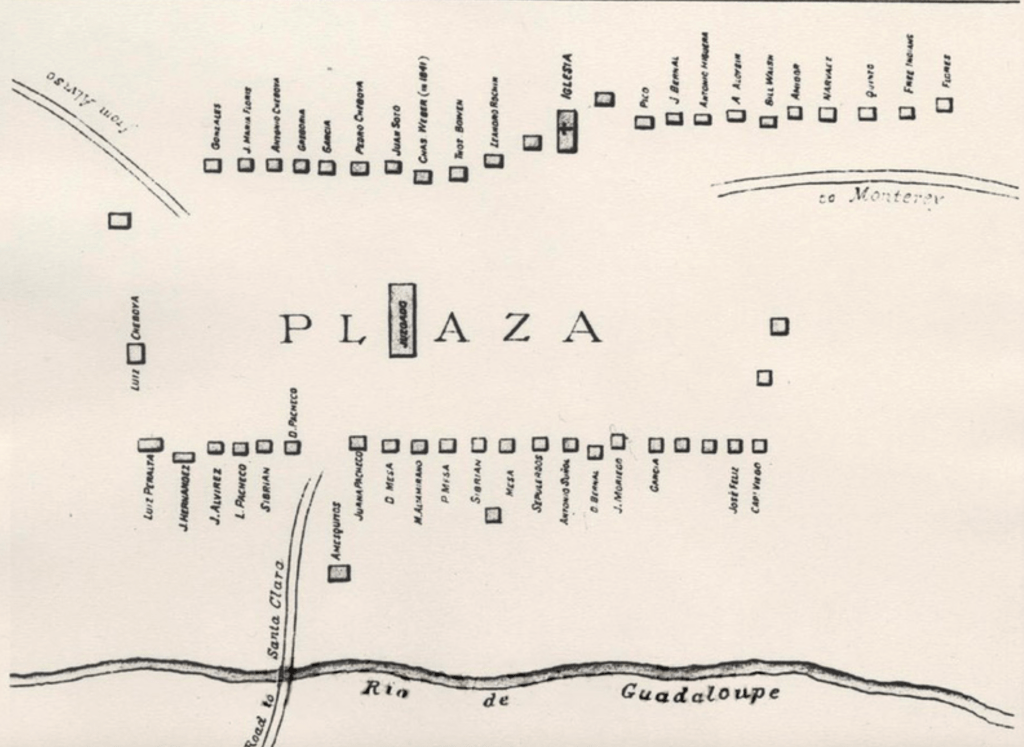
The Mexicans who founded San José, along with the avena barbata they brought for the journey, laid the foundation for the settlement during its first 73 years. The resilient pobladores (Mexican settlers) and their descendants built a community, governed themselves, and survived floods, drought, and conflicts with Americans who squatted on their land.
Just as slender wild oats disappear from the valley floor every summer, ethnic Mexicans vanished from 20th-century published historical works about San Jose. Much like how slender wild oat seeds nourish the soil, generating tall strands of green grass after the rain, ethnic Mexicans sustained the valley’s development as ranch hands, agricultural workers, and miners.
During the 1820s, Secundino Robles, a Mexican American landowner born in Santa Cruz, was the first non-Ohlone to see cinnabar embedded in the hillside soil. Cinnabar is a bright reddish-orange mineral that the Ohlone used for thousands of years as paint for ceremonial adornments.
During a visit to the Santa Clara Valley in 1845, Captain Andrés Castillero, a military officer from México City and a trained geologist, chemist, and metallurgist, inspected samples of the red rocks at Mission Santa Clara.
His experiments confirmed that the stones were cinnabar, a mercury-based mineral found in quicksilver mines. Quicksilver, another name for mercury, is a chemical used by miners to extract gold from rocks. Castillero formed a mining company named Santa Clara.
Castillero did not benefit from the Gold Rush, which brought riches to mine owners. He returned to México in 1847 to seek funding to expand his operations, and the Mexican government called him to duty during the 1846-48 U.S. War with México.
Castillero ultimately sold the Santa Clara mine. The new owner, the Quicksilver Mining Company, was a Pennsylvania-based organization that dominated the global mercury market. It named the location Cinnabar Hill and renamed the company New Almaden Mines.
Not long after the Quicksilver Mining Company arrived on Cinnabar Hill, structural racism again reared its ugly head in Santa Clara Valley. Company policies ensured that the miners were financially beholden to the Quicksilver Mining Company.
Immediately, the Company began charging residents $5 per month to rent the houses miners had built and occupied. The new owners replaced the general store with a company store that sold food at a 75% markup.
Inspired by the Mexican victory over French invaders in Puebla, Mexico, on May 5, 1862, miners began organizing and sharing ideas to resist the Company’s policies. In late 1864, miners and their families began protesting management.
In his groundbreaking book, A Devil in Silicon Valley: Northern California, Race, and Mexican Americans, Yale historian Stephen Pitti wrote, “This period of trial led to what may have been the earliest ethnic Mexican–organized labor activities in U.S. history.”
Even in the face of withering structural racism, the fight on Cinnabar Hill demonstrated the resiliency and perseverance of ethnic Mexicans in San José. Against all odds, the courageous miners stood in solidarity to defend their families and honor, as hardworking contributors to the economy that sustained San José and the surrounding area.
***
Note: La Raza Historical Society Publications anticipates that Mexican Heritage Plaza: A Symbol of Resilience and Perseverance will be available on March 21, 2026.
Stay tuned!